
Our dogs complete our lives. They’re our children. So, it was really difficult to not be able to be there with Lola. To our comfort, we knew our MSU family was with her.
Natalie Lachappell, Lola’s owner
Our dogs complete our lives. They’re our children. So, it was really difficult to not be able to be there with Lola. To our comfort, we knew our MSU family was with her.
Natalie Lachappell, Lola’s owner
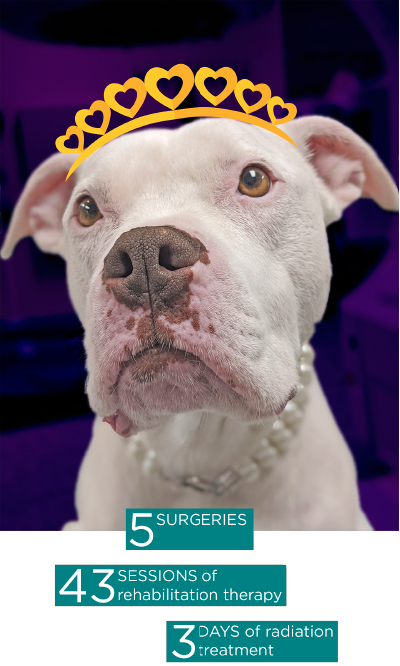
Many Spartans call Michigan State University their home away from home. Even Lola, an 8-year-old pit bull terrier, can’t seem to stay away from the land of the green and white. The smiley-eyed, pearl-wearing rescue pup has spent 5 years of her life in and out of MSU; 5 surgeries, 43 sessions of rehabilitation therapy (that’s 301 sessions in dog time!), and the 3 days it took to complete a full course of radiation treatment.
“If I had the option of taking my animals to any veterinary clinic—any I could—it would be MSU,” says Natalie Lachappell, Lola’s owner. “If we lived closer to Lansing, we would be there for everything. We’ve bonded with everyone, from the receptionists to the nurses and doctors. Lola’s obsessed with going to the vet. She wiggles her butt, gets squinty-eyed, and smiles. I love that she loves going to the vet; it’s made all this so much easier.”
Five years ago, Lola tore the cranial cruciate ligament (CrCL), the equivalent of the anterior cruciate ligament (ACL) in humans, in both of her knees. Her knees were repaired by her local veterinarian via modified retinacular imbrication technique (MRIT), and rehabilitation therapy was recommended to aid in her recovery. Based on a personal endorsement, Lachappell brought Lola to the Rehabilitation Service at the MSU Small Animal Clinic.
Only two months post-surgery, both MRITs failed, and Lola had two torn CrCLs—again. And she had to have surgery—again. Another veterinary clinic repaired Lola’s knees with a surgical procedure called tibial tuberosity advancement procedure (TTA), which they performed bilaterally in February of 2018. TTA aims to change the dynamics of the knee so that the torn ligament (the CrCL, in this case) is no longer necessary for joint stabilization.
Following her bilateral TTA surgery, Lachappell brought Lola back to MSU for rehabilitation—but she wasn’t progressing. That’s when Lachappell made an appointment for Lola to see Dr. Karen Perry, clinician for the Hospital’s Orthopedic Surgery Service. After Perry examined Lola and collected X-ray images of her knees, it was discovered that incorrectly sized equipment had been placed in both of Lola’s knees during the bilateral TTA procedure. As such, the surgery had failed to adequately stabilize her knees. This explained Lola’s lack of healing progress.
“At the time Lola presented to MSU’s Orthopedic Surgery Service, her left knee was substantially less stable than the right, which caused her a great deal of pain,” says Perry. “On top of that, bilateral surgeries are associated with higher complication rates. I felt Lola had suffered enough of those! So, I decided to operate on the left side first.”
The TTA previously performed was modified. Once the correct-sized implants were in place, Lola’s knee was immediately more stable and comfortable. So much so that unfortunately, Lola jumped from a sofa mid-recovery in December of 2018, and ruptured the caudal cruciate ligament (CCL) in that same knee (her left one)—and back to Perry’s operating table Lola went.
Perry performed a reverse MRIT procedure to place a prosthetic CCL and return Lola’s left knee to stability. “Initially, the plan was to operate on the right knee once Lola recovered from the surgeries on the left. However, following extensive physical rehabilitation, Lola was doing so well that surgery on her right knee was postponed indefinitely. We only wanted to subject Lola to another surgery if the pain associated with her right knee recurred,” adds Perry. “The character and resilience of both Lola and her family had us all falling in love with her every visit!”
Just as it seemed Lola was out of the woods as far as new injuries were concerned, another hurdle popped up in the spring of 2020—another hurdle in addition to the novel Coronavirus pandemic.
“We noticed that Lola was slower than normal,” remembers Lachappell. “She seemed winded and her belly was swollen. First, we thought she just put on a few pounds because she’s our treat monger. But it wasn’t a few extra pounds, it was cancer.”
Lola’s local veterinarian performed an ultrasound, which revealed a tumor and fluid around Lola’s heart and fluid in her belly. The veterinarian suggested for Lola to see a veterinary cardiologist. “Back to MSU we went,” says Lachappell. “In the midst of that horrific news, we knew there was no place we’d rather go.”
As if a cancer diagnosis wasn’t already complicated and stressful enough, COVID-19 presented a host of other issues for Lola and Lachappell. In Michigan, access to elective medical appointments was restricted. At the time, that included non-emergent veterinary services. Though Lola was able to be admitted to MSU’s Small Animal Emergency and Critical Care Medicine Service (ECCM) on an emergent basis, neither Lachappell nor her husband were allowed inside the Hospital throughout the duration of her week-long stay, per the Hospital’s revised operations that were implemented in March of 2020.

“Our dogs complete our lives. They’re our children,” notes Lachappell. “So, it was really difficult to not be able to be there with Lola. To our comfort, we knew our MSU family was with her.”
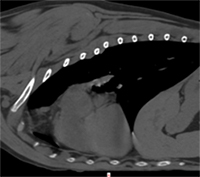
On Friday, April 17, Lola’s week-long stay at the Hospital began. On examination in the MSU Small Animal Intensive Care Unit, her heart and lungs sounded muffled, her heart rate was slightly faster than normal, and it seemed difficult for Lola to breathe. Based on these symptoms, the veterinary healthcare team was suspicious that Lola may have pericardial effusion (excessive fluid around her heart). Sure enough, the ECCM team collected diagnostic images (via focused assessment with sonography in trauma, or FAST scans) and found free fluid inside Lola’s abdomen and chest, as well as around her heart.
A total of 880 mL of blood-tinged, clear fluid was removed from the area around Lola’s heart and lungs; thankfully, no abnormal cells were noted by MSU’s clinical pathology team, a section located within MSU’s Veterinary Diagnostic Laboratory that monitors and diagnoses disease by examining blood, body fluids, and biopsy specimens. An echocardiogram revealed a tumor above the left atrial body that was compressing Lola’s heart and was at least 2.5 x 4.5 cm.
“Lola’s breed, the location of the tumor, and the findings of her echocardiogram were strongly suggestive of a chemodectoma, a type of heart-base tumor (HBT). The mass was producing fluid around her heart, causing a cardiology emergency known as cardiac tamponade. This condition causes heart failure and additional fluid to collect in the chest and abdomen,” notes Dr. Leanne Magestro, clinician for the Hospital’s Radiation Oncology Service.
Lola’s diagnosis was made based on diagnostic imaging only, which is common for tumors in this location. This is due to the tumor’s relative inaccessibility both at the center of the chest and near a critical organ, the heart. The majority of HBT are chemodectomas, which are cancers of the pressure-sensing cells in the blood vessels. Unfortunately, Lola’s tumor caused fluid to gather around her heart, which induced heart failure. This meant that surgical intervention and further cancer treatment would be necessary to save her life.


Lola didn’t fight for her life alone, though; visitors from the MSU Rehabilitation and Orthopedic Surgery services frequented her temporary residence in the Hospital often throughout that week. “To know there were people there who care so much about her, even though COVID complicated things, she wasn’t their patient at the time, and she isn’t their dog, was such a relief; that compassion provided the bit of extra support that we really needed during Lola’s week-long stay at MSU,” says Lachappell.
Due to the critical condition of her heart, Lola was transferred to the Hospital’s Cardiology Service for a surgical procedure known as a subtotal pericardiectomy. This surgery prevents pressure due to fluid buildup around the heart. Dr. Bari Olivier, chair of the MSU Department of Small Animal Clinical Sciences and co-interim director of the MSU Veterinary Medical Center, performed the surgery. During the surgery, Olivier attempted to sample the tumor, but was unsuccessful.
One month later, after Lola recovered from surgery, Lachappell brought her back to MSU for a CT scan and fluoroscopy (study of moving body structure; similar to an X-ray movie) of her chest so the tumor could be re-evaluated. Lola’s veterinary team wanted to make sure the tumor in her heart had not spread to other organs. They also wanted to determine how much the heart moved in the chest while it was beating and facilitate a plan for radiation therapy. Fortunately, there was no evidence of cancer in other organs, and there was very little fluid buildup in Lola’s chest cavity.
“Drs. Olivier and Magestro gave us so much light and hope in such a dark time—I can’t even put into words how amazing the team was. From emergency and cardiology, to radiation oncology, they treated Lola like one of their own,” says Lachappell.
After assessing Lola’s case, the MSU veterinary healthcare team opted for stereotactic radiation therapy (SRT). SRT is an advanced form of radiation technology that involves the application of hyper-focused high-dosed radiation over the course of a few days. For Lola’s treatment, SRT was conducted with the use of a technique known as volumetric modulated arc therapy (VMAT). VMAT is a novel radiation therapy that delivers radiation doses continuously as the treatment machine rotates (this machine is called a linear accelerator; the MSU Radiation Oncology Service operates a Varian Trilogy). With this targeted therapy, the shape of the tumor and the dosage needed are matched accurately, excluding the surrounding normal, non-cancerous tissues from radiation.
“Being able to talk to Dr. Magestro about our options was the light at the end of the tunnel,” says Lachappell. “She held our hands, guided us, and gave us hope that there was something we could do to fight this cancer. Because of her, we made a choice that was best for Lola, which was all that mattered.”
Lachappell brought Lola to MSU for SRT treatment from Tuesday, May 26 through Thursday, May 28. At each visit, Lola was placed under general anesthesia and positioned for radiation therapy. A cone-beam CT scan was performed to verify the location of her tumor and make certain all her normal organs were in the correct position before treatment. She recovered well each day, and even had time for a photoshoot or two!
Lola has since graduated from radiation therapy! “Moving forward, Lola should be able to resume living her best life at home. She will need a recheck cardiology evaluation and CT scan three- or four-months post-treatment to monitor her tumor and secure normal function of her heart,” says Magestro.
“Lola’s a fighter! Her resilience throughout this entire process has been incredible. She’s finally back to herself and playing like a puppy again. *Though this journey isn’t quite over, I look back on all the photos Dr. Magestro took and I can’t help but smile. I got one framed and personalized for her and her team, actually. That’s how above and beyond they went,” says Lachappell.

From months of rehabilitation therapy and a unicorn party, to an emergency surgery and a radiation-oncology-graduation photoshoot during the coronavirus pandemic, it’s safe to say that Lola will always be a special #SpartanDawg.
“This entire journey has been filled with many ups and downs—yet, we’ve felt so secure knowing that Lola has been in the absolute best hands. We couldn’t have asked for a better veterinary facility all around in every department,” says Lachappell. “I tried to put it into words as best as I can, but there’s just no way I can show my appreciation for how much MSU has done for us. From the bottom of my heart, I’m so grateful. You guys will always be our family, no matter what. I’ll always come to MSU.”
*Lola visited the Cardiology and Radiation Oncology teams four months after completing radiation therapy. Her owner reports that she has been feeling great at home. A recheck echocardiogram (heart ultrasound) revealed normal heart function. A recheck CT scan of the chest revealed a reduction in the tumor size by more than one third. This means that not only did radiation stop the tumor from growing, but relieved pressure on the heart and major blood vessels. Because these tumors (chemodectomas) tend to grow and shrink slowly, it is possible her tumor could continue to respond as time goes on. The MSU Cardiology and Radiation Oncology services will continue to see Lola for imaging and heart checks every 6 months.
