By Leanne Magestro, DVM, DACVR (RO)
Featuring H. Grady Bailin, DVM, BA; N. Bari Olivier, DVM, PhD, DACVIM
History and Presentation
Lola, an 8-year-old pit bull terrier, presented to the Michigan State University Emergency and Critical Care Medicine Service (ECCM) on Friday, April 17, 2020 for tri-cavitary effusion, or fluid within the abdominal, chest, and pericardial cavities. Her owner noted that she had been lethargic and bloated for several days. Lola’s additional medical history includes a long relationship with the MSU Orthopedic Surgery and Rehabilitation services for knee injuries.
On presentation, Lola was quiet, alert and responsive with pink mucus membranes. Her heart and lungs were muffled on auscultation, though her heart rate was slightly faster than normal, and she demonstrated effort while breathing. She had a marked fluid wave, consistent with abdominal effusion. Pulse oximetry was 91% (most patients are >98%). Both abdominal and thoracic FAST scan (focused assessment with sonography for trauma) were positive for fluid throughout the abdomen, chest, and around the heart.
Approximately 1 hour later, Lola’s mentation became dull and her mucous membranes were cyanotic (blue). A total of 880 mL of transudate (blood-tinged clear fluid) was removed from the area around her heart and lungs; no abnormal cells were noted by the pathologist. An echocardiogram was performed which revealed an at least 2.5 x 4.5 cm tumor over the left atrial body, compressing the heart.
Lola continued to develop fluid around the heart which required removal and placement of a pericardial catheter starting the next morning, Saturday, April 18.
Diagnosis
Lola’ s breed, the location of the tumor, and the findings of her echocardiogram were strongly suggestive of a chemodectoma which is a type of heart base tumor (HBT). The mass was producing fluid around the heart, causing a cardiology emergency known as cardiac tamponade, which causes heart failure and additional fluid in the chest and abdomen.
Treatment and Outcome
Lola was transferred to the Cardiology Service for a surgical procedure known as a subtotal pericardiectomy, which prevents pressure due to fluid buildup around the heart. During the surgery, an attempt to sample the tumor was made but was unsuccessful.
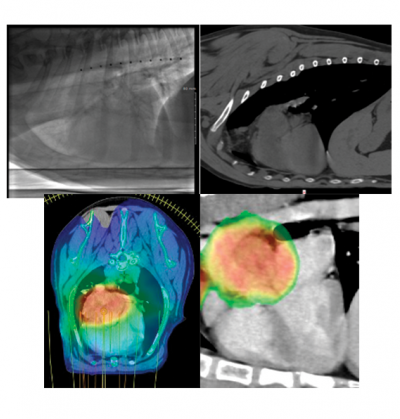
A month later, once Lola recovered from surgery, a CT scan and fluoroscopy of her chest were performed to evaluate the extent of the tumor. This was done to make sure the tumor had not spread to other organs, to facilitate a plan for radiation therapy, and determine how much the heart moved in the chest while it was beating. Fortunately, there was no evidence of cancer in other organs and there was very little fluid buildup in her chest cavity.
Due to many factors, Lola’s veterinary healthcare team felt that stereotactic radiation therapy (SRT) was the best choice of treatment for her. This protocol involves 1 treatment per day for 3 consecutive days, under general anesthesia; high doses of radiation are delivered to the tumor while using advanced technology to protect the nearby tissues. Her prescription was 10 Gray times 3 treatments, for a total of 30 Gray (the unit of radiation therapy prescriptions; 1 Gray = 1 joule per kilogram of tissue).

Lola was brought to MSU for SRT treatment from Tuesday, May 26 through Thursday, May 28. Each visit, she was placed under general anesthesia and positioned for radiation therapy. A cone-beam CT scan was performed to verify her tumor and make certain all her normal organs were in the correct position before treatment. A technique known as volumetric modulated arc therapy (VMAT) was used. She recovered uneventfully each day.
It has been approximately six weeks since Lola’s treatment, and her owner has reported that she is thriving at home. Lola will need a recheck cardiology evaluation and CT scan three–four months post-treatment to monitor her tumor and to secure normal function of her heart.
Comments
Lola’s diagnosis was made on imaging findings only, which is common for tumors in this location. The majority of HBT are chemodectomas, which are cancers of the pressure-sensing cells in the blood vessels. Breeds with short noses such as boxers, bulldogs and Boston terriers are most commonly affected, but they can occur in any breed. Generally, they are considered to be very slow growing tumors, progressing over months to years. Some dogs may live their entire lives with tumors and never have symptoms. Approximately 20% of patients develop spread of their cancer to other organs. Unfortunately, Lola’s tumor was making fluid around her heart and causing her heart to fail, which made treatment necessary to save her life.

Treatment of HBT in dogs is not thoroughly described. Surgical removal of a tumor in this location is considered high risk and thus is not routinely offered. There are currently three treatment options available: surgical pericardiectomy, radiation therapy, and an oral chemotherapy called toceranib phosphate (Palladia). Two studies have suggested that pericardiectomy can improve quality of life for dogs with HBT. Two additional studies and a case report suggest radiation therapy may shrink tumors. A single study on Palladia resulted in a perceived benefit by most pet owners but a measurable response in less than 30% of patients.
SRT requires specialized equipment and training and is not appropriate for every tumor or every patient. This is determined on a case-by-case basis. Treatment involves the delivery of high energy X-rays to a tumor with specialized anesthesia protocols. It is not painful for the patient to receive, nor does it leave them as radioactive. Potential side effects and a monitoring plan are discussed in detail with the owner prior to treatment. The goal of therapy is to stabilize or shrink a tumor and allow a patient to live as long as possible with excellent quality of life.



