New therapeutic tools may be on the horizon for patients with allergies, IBS, migraines, and other immune-triggered conditions.
In his latest paper, published in the Journal of Allergy and Clinical Immunology (JACI), Dr. Adam Moeser dives further into the mysteries that link the immune system to a multitude of common diseases and disorders. Clinical signs of irritable bowel syndrome (IBS), migraines, allergies, and other immune-triggered conditions are caused by an overreaction of the immune system; Moeser has discovered why that overreaction occurs.
“Mast cells express a receptor on their surface, the CRF2 receptor,” says Moeser, the Matilda R. Wilson Endowed Chair and an associate professor for the Department of Large Animal Clinical Sciences at the Michigan State University College of Veterinary Medicine. “We’ve discovered that the CRF2 receptor is a master regulator of mast cell activity. When the receptor is inhibited, mast cells overreact when they respond to normal cues, such as stress and allergens. That overreaction can cause exacerbated disease flare-ups.”
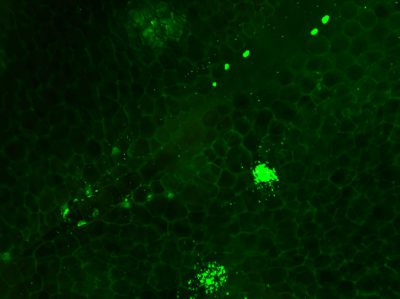
The process begins when mast cells—a specific kind of immune cell—receive a signal (an allergen, for example). Mast cells have intracellular stores of calcium and when they receive a signal, the cells dump these stores. This triggers a chain of events that causes the mast cells to take in large quantities of extracellular calcium.
The extracellular calcium influx launches a process in mast cells known as degranulation; during degranulation, cells release mediators, which are the mast cells’ immune response. For example, when a mast cell encounters an allergen, it would release the mediator called histamine. When enough degranulation has occurred to mitigate the original signal (in this case, the allergen), the CRF2 (corticotrophin releasing factor subtype 2) receptors signal for the mast cells to stop the degranulation process.
In a person with properly functioning mast cells, this is an effective process. The mast cells up- and down-regulate degranulation as needed. In a person who has encountered an allergen, mast cell degranulation (the release of histamine) would initiate mucus production, redness, inflammation, itchiness, and other signs and symptoms typical of allergic reactions.
But for some, the CRF2 receptors that exist on mast cells can be dampened, and thus have an impaired ability to control or limit degranulation. So, the mast cells continue to degranulate and become hyperactive.
Mast cell hyperactivity manifests as the clinical signs and symptoms of immune-triggered conditions. When mast cells overreact to an allergen, a person may experience anaphylaxis, which is a severe and potentially deadly allergic reaction. Another example involves mast cells in the gut that receive a stress-related signal in the form of neuropeptides. Overreaction there may cause signs and symptoms of IBS and other stress-related GI disorders.
This discovery, made through genetic and pharmacological research, may lead to biomarkers and pharmacological therapies that potentially could help flag and control the symptoms of allergies, anaphylaxis, IBS, migraines, and other related disorders by observing and therapeutically manipulating CRF2 receptors.
“Our next step is to determine how CRF2 senses and controls mast cell degranulation and how lifestyle factors (e.g., chronic stress) may affect CRF2 expression,” says Moeser.
JACI is the number 1-ranked journal in Allergy and number 6 (out of 150) in the Immunology category. It is considered a high-impact journal with an impact factor of 13.258. For more information on Dr. Adam Moeser and the Gastrointestinal Stress Biology Laboratory, visit the College’s website.
More information
Read the story from MSUToday and a piece written by Dr. Moeser for The Conversation.
