By Kathryn Winger, DVM, DACVIM (Neurology), Andrew Armstrong, DVM, and Sarah Shull, DVM, CCRT
History and Diagnosis
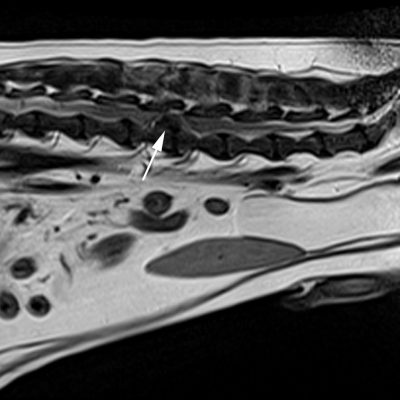
Ozzy, an eight-year-old male neutered Cockapoo, was presented to the MSU Veterinary Medical Center for an acute onset of paralysis. One day prior to presentation, Ozzy’s owners noticed that he was not defecating and had a mild right pelvic limb lameness. By the following morning, Ozzy was paralyzed in both pelvic limbs. A thorough neurological examination was performed by Dr. Andrew Armstrong which revealed that Ozzy was paraplegic with a decreased patellar reflex on the right and no deep pain perception. The loss of pain perception is an indicator of a very severe spinal cord injury. Immediate action was needed. An MRI of Ozzy’s spine identified a disc extrusion at the level of his third and fourth lumbar vertebrae. This was causing spinal cord compression.

Treatment and Outcome
With the assistance of Dr. Kathryn Winger, assistant professor of Neurology and Neurosurgery, a decompressive hemilaminectomy to remove the extruded disc material and decompress the spinal cord was performed. Following surgery, small neurological improvements were seen daily, including the return of deep pain perception, mild motor function in the left pelvic limb, and the return of minimal urinary continence. Despite the clinical improvement, Ozzy’s owners were prepared for a slow recovery, as well as expectations for life-long neurological impairment and urinary incontinence.
Dr. Winger recommended rehabilitation for Ozzy’s continued improvement. Using a multimodal approach, Ozzy’s rehabilitation therapy began while he was still in the Hospital. In addition to his round-the-clock care in ICU, he received daily targeted neurologic retraining exercises and laser therapy from Becky Rathbun, LVT, from the Rehabilitation Service, and acupuncture from Dr. Elizabeth Carr. Prescribed exercises were performed by Ozzy’s owners daily when he returned home.
Two weeks after surgery, Ozzy returned to MSU to begin further in-clinic rehabilitation. He visited the Dr. Elwood and Linda Collins Rehabilitation Center for nine sessions over the following three months, which started as weekly visits and tapered off to every other week. His sessions included hydrotherapy in the underwater treadmill, therapeutic laser over his surgical site, and strengthening and body-awareness exercises. Three more acupuncture treatments were performed during this time. Ozzy showed weekly progression and his exercises advanced in difficulty each session.


The Neurology Team monitored Ozzy’s status with frequent visits during his therapy. When he completed rehab, Ozzy was able to easily perform his exercises of sit, stand, and down transitions, weaving between cones, walking over cavaletti boards, and walking backward and to the side, as well as various types of balance work. His final underwater treadmill session consisted of a 30-minute walk at 0.8 mph, totaling 692 yards.
Ozzy’s outcome was very favorable, as he regained full motor function and continence with very minimal deficiencies. His recovery was made possible by diligent owners, advanced diagnostics, proper surgical treatment, and the collaboration of multiple services.
Comments
In cases of intervertebral disc extrusion where deep pain perception has been lost, approximately 50% of patients will regain ambulatory function with surgical intervention. Clinically, a better outcome is expected in dogs with loss of deep pain perception for less than 24 hours prior to surgery as compared to those dogs without deep pain perception for more than 24 hours. Another prognostic indicator is the return of deep pain perception within the first two weeks post-operatively. Unfortunately, without surgical intervention, prognosis for return of ambulatory function is poor.



