Read More
Read More
Ballet dancers, football and rugby players, basketball and soccer players, equine athletes, and companion dogs—all have benefited from the scientific discoveries and clinical applications generated in Dr. Steven Arnoczky’s Laboratory of Comparative and Orthopaedic Research (LCOR).
The innovative work of Arnoczky, the Wade O. Brinker Endowed Professor of Veterinary Surgery, honors and builds on the legacy of Wade O. Brinker, considered the father of veterinary orthopaedic surgery. As the first Wade O. Brinker Chair, Arnoczky has, along with his collaborators and students, changed the course of human and animal medicine for 25 years.
Brinker brought new technologies and techniques to veterinary medicine and was a mentor to some of the profession’s most noted small animal surgeons. In the same vein, Arnoczky has focused his research career on developing new and innovative techniques in the field of orthopaedic surgery, as well as improving existing methods. Arnoczky’s work has focused on improving human health, always with the idea of honoring Dr. Brinker’s legacy.
Two of Arnoczky’s most important contributions to science are his work on the anatomy of the meniscus and his focus on overuse tendon injuries.

Veterinary Science and a Revolution in Human Orthopaedic Medicine
Every knee has two menisci—pads of tissue that absorb shock, distribute weight load, and provide structural integrity to the knee. Until the late 1970s, damaged (torn) menisci were removed, in part or in total, simply based on the misconception that these tissues were unable to heal due to a lack of a blood supply. Because of the negative sequella (cartilage damage, osteoarthritis) associated with meniscectomy, there was a desire within the orthopaedic community to focus on preserving these structures whenever possible.
“Since I was unable to find any published reports on the blood supply of the menisci in humans, we undertook a study to investigate this,” said Arnoczky. “What we found was that the menisci do have a robust blood supply, albeit limited to the periphery of the structure.” This finding led to the concept that tears within this vascular zone were indeed able to heal, which, in turn, led to a worldwide change in the standard of care—repairing injured menisci rather than removal, whenever possible.
Arnoczky and his colleagues developed a classification system used to determine which meniscal tears can be repaired. He identified three zones in the meniscus: red, which is vascular and has an excellent healing prognosis; red-white, which is at the border of vascular supply and has a good healing prognosis; and the white, which is relatively avascular and has a poor prognosis for healing. Arnoczky’s classic slide illustrating the blood supply of the human medial meniscus is said to be the most viewed picture in all of orthopaedics.
“Steven’s work on meniscal anatomy and meniscal blood supply significantly altered the approach of orthopaedic surgeons to meniscal repair,” said Jo Hannafin, professor of orthopaedic surgery at the Weill Medical College of Cornell University Sports Medicine and Shoulder Service at the Hospital for Special Surgery.
An Archeology of Discovery: Research Awards
For his groundbreaking discovery and classification of the vascularity in menisci, Arnoczky became the second non-physician to receive the O’Donoghue Award for Sports Medicine Research, given by the American Orthopaedic Society for Sports Medicine. This was his first of two O’Donoghue Awards and just one of what have been dozens of prestigious awards usually given to physicians.
Tracking the awards Arnoczky and the LCOR lab have received is one way to map his contributions to orthopaedic surgery.
Meniscal Transplants
Arnoczky’s work in the early and mid-1980s identified ways to preserve cadaveric menisci for transplantation and demonstrated the ability of these transplants to heal within the recipient’s knee and function normally. As a result of these findings, by the end of the decade, orthopaedic surgeons were routinely repairing torn menisci or replacing severely damaged menisci with meniscal transplantation.
The American Orthopaedic Society for Sports Medicine recognized LCOR’s contributions in this arena with the 1986 and 1987 Cabaud Awards for Soft Tissue Research in Sports Medicine and the 1991 Excellence in Research Award. The Cabaud Award recognizes studies that best exemplify clinically relevant laboratory basic science research.
Tissue Engineering
In the early 1990s, the concept of tissue engineering began to emerge in orthopaedic surgery. The idea that an absent or severely damaged connective tissue could be encouraged to regenerate in the body through the addition of an engineered scaffold would be a game-changing advancement, especially in cases of rotator cuff injury, where the torn tissues are often degenerated and difficult to repair. Arnoczky and his colleagues at LCOR conducted a study that examined whether an implant of porcine small intestinal submucosa would stimulate the regeneration of a rotator cuff tendon in a canine model. The team found that the implants represented an exciting alternative to existing tendon repair procedures, especially when the patient had degenerative tissues or large rotator cuff defects.
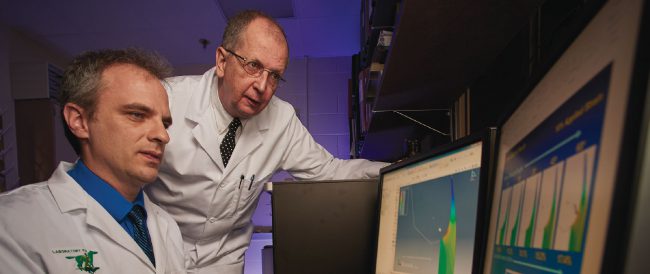
For this work, Dr. Arnoczky’s LCOR team, including his then-student and current colleague, Dr. Loïc Déjardin, was recognized with a second O’Donoghue Award in 2000.
Preventing Transmission of the HIV Virus

Preventing the spread of a retrovirus like HIV is not an accomplishment many orthopaedic researchers can claim. But a study that Arnoczky considers one of his most important accomplished exactly this.
In the early 1990s, there was speculation that freeze-drying bone grafts infected with a retrovirus would render them noninfectious. This speculation was based on a study that found recipients of freeze-dried bone grafts from a donor infected with HIV all tested negative for the virus. Meanwhile, 75 percent of the patients who received fresh-frozen bone from the same donor contracted the HIV virus.

This sort of scientific leap leaves wide gaps in knowledge, something that draws Arnoczky’s attention. He set out to conduct the first rigorous investigation into whether freeze-drying would inactivate infected connective tissues. The feline leukemia virus is a retrovirus widely used as an animal model for HIV. LCOR tested to see if connective tissues from feline leukemia-infected donors were transmittable and if freeze-drying procedures used at the time could prevent this. Dr. Arnoczky worked with Dr. Cheryl Swenson, an expert in feline virology at MSU, and determined that a retrovirus could, in fact, be transmitted through connective tissues. This discovery led to sterilization and donor screening procedures in human tissue banks to prevent the transfer of retroviruses, including HIV. This life-saving contribution was recognized by the American Orthopaedic Society for Sports Medicine with the 2004 Cabaud Award, Arnoczky’s third.
Biomaterial Testing and Computational Biology
One of LCOR’s laboratories is the Biomaterial Testing and Computational Biology Laboratory. The lab’s biomaterial testing includes determination of the kinds of changes that occur in tendons, skin, and implants after various treatments. Their computational work includes investigations to explain experimental results.They also provide data and statistical analysis for the studies performed in the lab.
“We were able to show why people get tendinopathy in their patellar tendon by using a finite element computer model,” said Arnoczky. “My research colleague and former graduate student, Dr. Michael Lavagnino, designed a finite element model that showed why the injury occurs where it does.”
In addition, the team designed a second study using this model to test orthotics (straps and bands) that could be used to prevent the injury.
“Dr. Arnoczky always takes the basic science research and tries to show its clinical relevance,” said Lavagnino.
This work was recognized by the American Orthopaedic Society for Sports Medicine with the 2008 Cabaud Award, LCOR’s fourth, and the 2012 T. David Sisk Award for Best Original Research Paper from the American Orthopaedic Society for Sports Medicine.

Recognition
“What I have always told our students is that creating an original idea is the most important, and often most difficult, aspect of any research project,” said Arnoczky. “While it is important to think outside the box, it is more important to make sure your research is novel, has clinical application, and is translatable.
In 2014, Dr. Arnoczky was recognized by the Orthopaedic Research Society as a Pioneer of Innovation, a distinction that recognizes scientists whose sustained research in biological, engineering, or clinical sciences have translated into novel therapies and improved patient care.
Arnoczky’s research was also noted in an article from the Journal of Bone and Joint Surgery entitled “The Hundred Most-Cited Publications in Orthopaedic Knee Research.” The list spanning 50 years of orthopaedic knee research included two publications from Dr. Arnoczky’s lab.
“Dr. Arnoczky’s work was probably the single most important factor that led me to pursue a clinician-scientist career,” said Dr. Scott Rodeo, former head of Sports Medicine at the Hospital for Special Surgery and co-author of one of the cited publications. “He has carried out elegant and deeply insightful studies into the biology of tendon, ligament, and meniscus that have direct clinical relevance.”
Perhaps the most notable recognition of the impact of Arnoczky’s research on clinical orthopaedic practice was his election to the American Orthopaedic Society for Sports Medicine Hall of Fame. This, the Society’s highest honor, recognized Arnoczky’s basic contributions to the advancement of ligament reconstruction of the knee and meniscal repair and replacement. Arnoczky is the second non-physician to receive this honor.
“This extraordinary honor for Dr. Arnoczky reflects the medical community's recognition of his contributions to orthopaedic medicine," said Dr. John Baker, dean of the MSU College of Veterinary Medicine. "It speaks to his accomplishments in basic science and comparative research.”
Framing a Research Question
“I have always tried to make sure that every student who passes through our lab appreciates what Dr. Brinker has done for the College, for MSU, and for the veterinary profession. It is important for them to understand his legacy.”
This Albert Einstein quote hangs on a wall in the LCOR laboratory:
“Imagination is more important than knowledge.”
“What I have always told our students is that creating an original idea is the most important, and often most difficult, aspect of any research pro-ject,” said Arnoczky. “While it is important to think outside the box, it is more important to make sure your research is novel, has clinical application, and is translatable. Finding the technology and expertise to accomplish the idea is the easy part.”
“Indeed, it is this approach that has allowed our original research in ligament and meniscal healing and transplantation to evolve from novel, clinically based concepts to the current standard of patient care in human orthopaedics,” said Arnoczky.
Arnoczky’s mentors conveyed to him the importance of novel, clinically relevant, translatable research. Those mentors include Dr. John L. Marshall and Dr. Wade O. Brinker.
Marshall received his DVM from Cornell University and practiced at Belmont race track in New York before going on to medical school. He was an orthopaedic resident before becoming the head of Sports Medicine at the Hospital for Special Surgery, the orthopaedic specialty hospital affiliated with New York Hospital and the Cornell University Medical College.
Arnoczky began his work in comparative orthopaedic research in Marshall’s lab. Arnoczky said of meeting Marshall, “It was simply the most transforming experience of my career.” After three months in Marshall’s laboratory of comparative orthopaedics, Arnoczky said he knew this was the kind of research he wanted to do. That was in 1974.
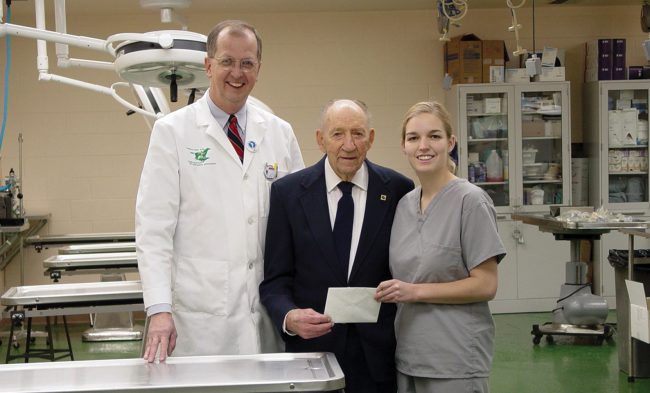
In 1976, Arnoczky formally met Brinker when delivering his very first research paper at the Veterinary Orthopaedic Society. “I hoped it was a good paper and was thrilled when Dr. Brinker complimented me on the work. He was such a gentle and caring man who was always so encouraging to young surgeons. I often think I could have read the comics from the newspaper and if Dr. Brinker would have said, ‘You read the funny papers well,’ I would have been just as proud. He was very special that way.”
That set up a lifelong relationship. It was 16 years later that Arnoczky joined the MSU College of Veterinary Medicine as the Wade O. Brinker Endowed Professor of Veterinary Surgery. Arnoczky said he was influenced by Brinker’s skill as a researcher and a mentor.
Arnoczky takes seriously the importance of mentoring scientists. Students say the way in which he frames a question and develops a project is one of the most important skills they learn.
“Professor Arnoczky has a great ability to shape a superior hypothesis in biology,” said Kenji Shirakura, a postdoctoral fellow supervised by Arnoczky in 1994. “He taught me that excellent scientists are those who have reasonable, extraordinary, and unique hypotheses. He helped me shape such a hypothesis and methodology for my study.”
Shirakura’s research on tendons’ reaction to stimulation had an important influence on the way ligament surgery is performed. Now professor at the Gunma University Faculty of Medicine and director of the rehabilitation center at Fukui-en Saiseikai Hospital, he is involved in research not only of motor organs but also of the central nervous system and disorders including Parkinson’s and depression.
Honoring a Legacy of Achievements
“Dr. Brinker’s legacy in veterinary surgery will always be framed by his numerous, original contributions to orthopaedics and his special dedication to mentoring,” said Arnoczky. “As the first Wade O. Brinker Chair in Veterinary Surgery I felt that my most important duty was to honor that legacy. I hope I was able to accomplish this.”
Indeed, Arnoczky’s career at MSU has honored and built on that legacy.
In 2010, Arnoczky received the Jacob Markowitz Award for Outstanding Surgical Research from the Academy of Surgical Research. He was only the second veterinarian to win this award. The first was Brinker.
In 2011, Arnoczky was the recipient of the American College of Veterinary Surgeons Founders’ Award, which recognizes diplomates who have made significant contributions to the development and teaching of surgical techniques and methodologies. He was the sixth ACVS Diplomate to be so honored. The first was Dr. Brinker.
Arnoczky’s students have won awards for their research at the local, state, and national level.
“I have always tried to make sure that every student who passes through our lab appreciates what Dr. Brinker has done for the College, for MSU, and for the veterinary profession. It is important for them to understand his legacy.”
The Bridge that Unites Human and Veterinary Medicine
Arnoczky talks about the importance of communication between physicians and veterinarians. His influence on that relationship resulted in his 1989 election into the American Academy of Orthopaedic Surgeons in recognition of the importance of his contributions and veterinary research to the field of sports medicine.
About 95 percent of Arnoczky’s presentations are at human orthopaedic meetings and he is often mistaken for an MD. He has been asked why he doesn’t go to medical school. Arnoczky responds by explaining that he is proud of his veterinary education and the unique perspective it brings to his research.
“Indeed, my veterinary training has allowed me to easily travel back and forth on the bridge that unites human and veterinary medicine. Something that Dr. Brinker started years earlier. A special memory that highlights this happened at one of the first human orthopaedic meetings I spoke at. After the lecture, an orthopaedic surgeon came up to me and told me of a veterinarian he met many years earlier who taught him how to plate a broken bone. He said the veterinarian was ‘one of the most skilled surgeons he had even seen and probably the best teacher he ever had.’ I immediately began to smile and said, ‘I bet his name was Wade Brinker.’ The surgeon said, ‘Yes, how did you know?’ ’It could only have been Dr. Brinker,’ I said.”