You might have called her “Abbey the Athlete.” Abbey was an active cat, used to long 10-acre walks with her owner, Ms. Martin, and jumping between perches at home. But at age nine, Abbey started to slow down.
“I noticed she was climbing stairs much more slowly than she used to, and jumping up and down on perches seemed awkward and clumsy,” said Ms. Martin. “It became apparent that Abbey was struggling to get around, much more than a normal cat would.”
After 2 years of medical treatment, and now 11 years old, Abbey’s quality of life hadn’t improved enough.
“My biggest concern for Abbey was that she was in pain,” said Ms. Martin. “I was worried that eventually she may be debilitated by her pain to the point that she would not be mobile at all. I wanted her to have a long, happy, pain-free life, enjoying all the activities that cats like to do.”
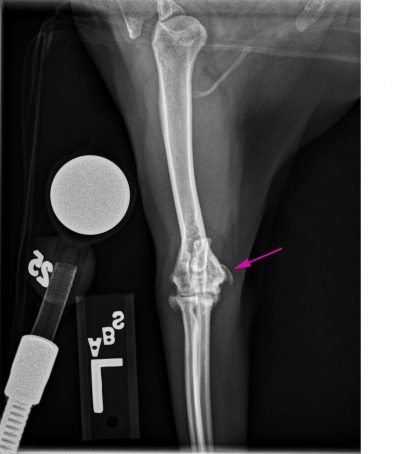
Ms. Martin knew it was time to consider other options. Ms. Martin and Abbey met with Dr. Sarah Shull of the Rehabilitation Service and then Dr. Karen Perry from the Orthopedic Surgery Service at the MSU Veterinary Medical Center. After diagnostic radiographs, Dr. Perry diagnosed Abbey with medial humeral epicondylitis (MHE). It occurs when mineral deposits develop around the elbow joint. When large quantities of the mineral deposits accumulate, they can cause nerve compression. These deposits may cause severe pain and often do not respond to conventional medical therapy.
“For so long, I didn’t know exactly what was wrong with Abbey,” said Ms. Martin. “During our first visit with Dr. Perry, she was able to immediately diagnose the source of Abbey’s limping and pain and discuss options based on the limited research available.”
The research was limited because Abbey’s joint condition is relatively unknown and unstudied in the veterinary community. Veterinarians suspect that MHE occurs due to repetitive injury, but it is difficult to recognize and often misdiagnosed. Dr. Perry is working to change that through her own research and by raising awareness while supporting patients struggling with the disease.

“She is so knowledgeable, and is able to share complex information in a way that is easy to understand,” said Ms. Martin. “Throughout the whole process, she discussed what to expect, kept me informed of the progress, and quickly answered any questions that came up along the way.”
Ultimately, surgery proved to be Abbey’s only option for improved quality of life. First, Dr. Perry removed the mineralized bodies and sections of tendon and muscle tissue that were causing nerve compression. Then she repaired the defect by reattaching the debrided tendons and muscles to the surrounding, healthy structures. The surgery immediately improved Abbey’s level of comfort.
After surgery, Abbey started working with Dr. Sarah Shull at MSU’s Dr. Elwood and Linda Collins Rehabilitation Center. Abbey started with laser therapy, icing, passive range of motion exercises, and acupuncture. At four weeks post-surgery, she began massage and walking on the underwater treadmill to build strength and mobility.
“When I drop Abbey off for rehab, I never have any concerns about Abbey being scared, in pain, or working too hard,” said Ms. Martin. “Dr. Shull makes sure that Abbey feels comfortable and is happy in rehab.”

Now, Abbey is enjoying life at home with Ms. Martin.
“Abbey is an entirely different cat than she has been for the past two years,” said Ms. Martin. “Her severe limp is much improved, and now is just barely noticeable. She is doing more jumping, stair climbing, and walking every day. The biggest change I have seen, however, is in her attitude. I love the confidence she now has. Dr. Perry, Dr. Shull, and the Rehabilitation team have accomplished what we set out to do: improve Abbey’s quality of life so she can be a normal cat again, pain-free and happy.”
Ms. Martin attributes much of Abbey’s success to the teamwork between Drs. Shull and Perry and the Rehabilitation team.
“I believe the effort from both clinicians made a huge difference in Abbey's outcomes following surgery,” said Ms. Martin. “Together, they diagnosed Abbey and developed the treatment plan. All along, they worked together as a team to facilitate Abbey's recovery—something truly unique about our experience with MSU.”



