By Marc Kinsley, DVM, MS, DACVS
History and Diagnosis
Levi, a 10-year-old paint gelding, presented to the MSU Equine Surgery Service with a traumatic puncture wound to the right axillary region that communicated with his chest cavity. Levi’s referring veterinarian administered a dose of Banamine and sedated Levi in order to evaluate the wound. Upon evaluation, the wound was found to communicate with the chest cavity, and lung tissue was palpable within the wound. With the help of local lidocaine blocks to the skin surrounding the wound, Levi’s primary veterinarian was able to place an air-tight stint bandage that prevented any further air from entering Levi’s chest cavity. Levi was then immediately referred to the MSU Veterinary Medical Center for further treatment.
At MSU, Levi presented as alert and responsive to Drs. Marc Kinsley and Jarrod Troy. The applied stint bandage was removed and the wound was evaluated. A large laceration and puncture wound was observed in the ventral axillary region on his right side with significant swelling and a large communication with the chest cavity. A number of mild skin lacerations also were noted on both front fetlocks and the lateral right hind limb. Pulmonary auscultation revealed decreased lung sounds in the caudodorsal lung field bilaterally. Subcutaneous emphysema was palpated throughout the chest, shoulders, and neck bilaterally.
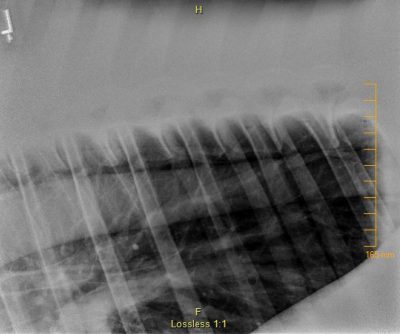
Drs. Kinsley and Troy further examined the thoracic wound, which extended through subcutis and underlying soft tissue, penetrating through the fifth and sixth ribs and communicating with the thoracic cavity. Thoracic ultrasound revealed a bilateral pneumothorax.
Treatment and Outcome

To combat Levi’s respiratory distress, Drs. Kinsley and Jamie Kopper placed indwelling chest tubes bilaterally to suction the air off of his chest cavity that was preventing him from being able to breathe normally. Levi’s thoracic puncture wound was debrided and cleaned using diluted Betadine solution. The wound was then packed with stallion-packing soaked in diluted Betadine and Vaseline, and finally wrapped with Elastikon. This resolved Levi’s respiratory distress for two hours, after which he developed clinical signs and was placed on continuous suction using a Thora-seal apparatus. Levi also was placed on IV antibiotic therapy (Procaine Penicillin G and Gentamicin) to prevent further infection and anti-inflammatory therapy (Banamine) to reduce inflammation and manage pain. Levi responded very well to continuous suction and his condition remained stable.
After showing no signs of respiratory distress, Levi was taken off continuous suction three days later. He was closely monitored and developed very limited clinical signs of respiratory dysfunction. His chest tubes were removed two days later when thoracic radiographs did not show evidence of pneumothorax bilaterally.
The wound continued to be cared for daily and Levi was closely watched for any signs of respiratory distress. In the absence of those signs, plans were made for Levi’s eventual departure from the Hospital. Levi was transitioned from injectable antibiotics to oral antibiotics and his wound was left open to see if it had healed enough to prevent a pneumothorax from occurring. In the 24 hours following the challenge, Levi was noted to have an increase in his inspiratory effort. Ultrasound at that time confirmed a pneumothorax. The wound was again packed and two 14-gauge catheters were placed and the pneumothorax corrected. With the wound packed, Levi showed no signs of respiratory distress and continued on the path to recovery over the seven days prior to being discharged from the Hospital.
Comments
Levi’s puncture wound and bilateral pneumothorax were severe, making fast-action from Levi’s primary veterinarian to prevent more air from entering the chest cavity all the more vital to Levi’s wellbeing. When a pneumothorax occurs, it prevents normal lung expansion. This leads to collapse of the lung, lack of oxygen, and potentially death. Applying the air-tight stint bandage allowed Levi to still maintain some oxygenation and survive the transport to Michigan State University. Without this life-saving action, Levi may not have had the successful outcome that was achieved. Once at Michigan State, the thoracotomy tubes that were placed, allowed for drainage of the remaining air from within the chest and allow for normal expansion of the lungs and oxygenation.



