By the MSU Comparative Opthalmology Service.
History and Presentation

Captain, a 3-year-old male neutered American Bulldog, first presented to MSU’s Comparative Ophthalmology Service in September 2018 with a 2-week history of a squinting, red, and blue appearing left eye (OS). Intraocular pressures (IOPs) were 72 mmHg in OS and 22 mmHg in the right eye (OD). While the examination of OS was limited by the severe corneal edema, the Ophthalmology team could appreciate optic nerve head atrophy and cupping, consistent with permanent, irreversible damage and vision loss. Examination of OD revealed the presence of multiple uveal cysts, and gonioscopy showed pectinate ligament dysplasia.
These combined findings resulted in the diagnosis of suspected primary angle-closure glaucoma (PACG) OS with OD possibly being in an early stage of glaucoma with IOP in the low 20s mmHg. An aqueous paracentesis was performed OS to lower the IOP, and medical treatment was initiated with latanoprost 0.005% ophthalmic solution q8h OS, dorzolamide 2%/timolol 0.5% ophthalmic solution in both eyes (OU) q8h, and systemic pain medication with oral gabapentin.
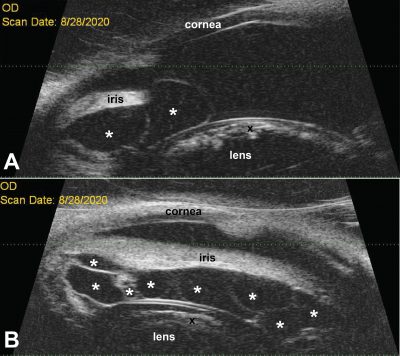
Because of poor response to therapy with the persistence of ocular hypertension, OS was enucleated by the Hospital’s colleagues at Town and Country Animal Hospital in Charlotte, MI. Captain’s OD was monitored closely over the next 21 months and treated with dorzolamide 2%/timolol 0.5% ophthalmic solution for IOP control and glaucoma prophylaxis as well as neomycin/polymyxin B/ dexamethasone 0.1% ophthalmic suspension for low-grade anterior uveitis with the intermittent appearance of trace flare and/or few cells in the anterior chamber. Over this time period, the IOP was maintained mostly between 20–25 mmHg, but the uveal cysts increased in size, pushing the iris anteriorly, resulting in a narrowing iridocorneal angle. At the same time, a cataract formed and slowly progressed. In June 2020, the uveal cysts were aspirated under general anesthesia by aqueous paracentesis using a 30G needle in order to flatten the iris and open the iridocorneal angle.

Diagnosis
Captain’s eye(s) were diagnosed with primary glaucoma OU, pectinate ligament dysplasia OD, uveal cysts OD, anterior uveitis OD, and cataract OD.
Treatment and Outcome
Because the cataract continued to progress with the deterioration of eyesight, Captain’s owners opted for him to have cataract surgery performed by phacoemulsification, knowing that glaucoma could worsen following surgery. The procedure was performed in September 2020. Phacoemulsification and placement of an intraocular lens (IOL) were combined with mechanical deflation of remaining uveal cysts, and endolaser cyclophotocoagulation for partial destruction of the ciliary body epithelium to reduce aqueous humor production and aid with IOP control. The surgery was followed by routine post-operative care and medication, including the continued use of topical glaucoma eye drops as well as tapering doses of topical and systemic anti-inflammatory medications and antibiotics. Since surgery, the IOP has been well-controlled (<15 mmHg), and Captain’s eyesight has improved.
Response to treatment in American Bulldogs with cysts and glaucoma is generally poor as seen in Captain’s first eye. MSU’s Ophthalmology Service is pleased with how well the second eye has responded to the combination of cataract surgery andendolaser cyclophotocoagulation. Unless secondary in nature, there is no cure for glaucoma and treatment is limited to lowering IOP by medical and surgical treatments. The Service will continue to monitor Captain’s eye very closely and consider additional medical and surgical treatments to preserve his sight for as long as possible.
Comments

Glaucoma is classified by primary vs. secondary. Captain is suspected to be affected by primary glaucoma based on the gonioscopically observed pectinate ligament dysplasia OD and the acute, severe increase in IOP OS. Furthermore, no underlying disease process, such as chronic anterior uveitis or intraocular neoplasm, could be identified that would have caused the bilateral glaucoma.
Uveal cysts are a common coincidental finding in dogs of certain breeds. In general, they are not of concern, unless their location and size inhibit the animal’s eyesight. In American Bulldogs, such as MSU’s patient, Captain, the uveal cysts may contribute to primary glaucoma development via a volume-effect, profound anterior chamber shallowing, and narrowing of an already abnormal, dysplastic iridocorneal angle. Furthermore, the cysts may cause a chronic, low-grade anterior uveitis and formation of a pre-iridal fibrovascular membrane, another common contributor to canine glaucoma development.
Most cataracts in dogs are considered primary or genetic. This also is possible for Captain; however, the chronic, low-grade anterior uveitis induced by the cysts may have resulted in secondary cataract formation. The combined surgical removal of the cataractous lens and the cysts allowed the flattening and posterior movement of the iris, thereby deepening the anterior chamber and opening the iridocorneal angle. This helped with the drainage of aqueous humor from the anterior chamber. Endolaser treatment of the ciliary processes resulted in lower production of aqueous humor. The combination of increased drainage and decreased production of aqueous humor achieved by our surgery resulted in an effective reduction of IOP.
Additional References Co-authored by MSU’s Faculty Members
Komáromy AM, Bras D, Esson DW, Fellman RL, Grozdanic SD, Kagemann L, Miller PE, Moroi SE, Plummer CE, Sapienza JS, Storey ES, Teixeira LB, Toris CB, Webb TR. The future of canine glaucoma therapy. Vet Ophthalmol. 2019 Sep;22(5):726-740. doi: 10.1111/vop.12678. Epub 2019 May 20. PMID: 31106969; PMCID: PMC6744300.
Pumphrey SA, Pizzirani S, Pirie CG, Needle DB. Glaucoma associated with uveal cysts and goniodysgenesis in American Bulldogs: a case series. Vet Ophthalmol. 2013 Sep;16(5):377-85. doi: 10.1111/vop.12000. Epub 2012 Oct 30. PMID: 23110479.
We thank our colleagues at Town and Country Animal Hospital in Charlotte (MI) for referring Captain to MSU’s Comparative Ophthalmology Service. It has been a privilege to work with him and oversee his ocular treatment.



