
History and Presentation
Dom, a 1.5-year-old English Springer Spaniel, presented to the MSU Veterinary Medical Center’s Soft Tissue Surgery Service for a previously diagnosed diaphragmatic hernia.
Preceding his diagnosis, Dom was evaluated by his primary veterinarian after experiencing an episode of acute respiratory distress (including vomiting, diarrhea, and lethargy). Thoracic radiographs showed a portion of his liver within the thoracic cavity, and he was diagnosed with a congenital diaphragmatic hernia. He was referred to MSU for a consultation.
Diagnosis
On presentation, Dom was bright, alert, and responsive with some visible signs of anxiety. His temperature and pulse were within normal limits, and he was panting heavily with normal respiratory effort. He had decreased lung sounds in the right caudal thorax and it was difficult to auscultate his heart. However, overall, he appeared to be comfortable, clinically well, and well-conditioned.
Radiographs were performed to assess the severity of his hernia and determine the exact location and diagnosis. The images showed a severely enlarged cardiac silhouette due to a suspected pericardial peritoneal diaphragmatic hernia (PPDH) with numerous abdominal organs in the pericardial sac (including colon, small intestines, and liver). Due to the severity of the hernia and number of organs located within the pericardium leading to severely decreased lung capacity, immediate surgical treatment was recommended to prevent acute complications.
Dom stayed overnight in preparation for exploratory laparotomy and PPDH repair. Dom was comfortable overnight and breathed well with some vomiting, which was treated with Cerenia.
Treatment and Outcome
Surgeons planned a PPDH repair via a ventral midline celiotomy approach. He was placed in dorsal recumbency, prepped, and draped routinely.
A ventral midline incision from xiphoid to just cranial to the prepuce was made using a 10# blade. The linea alba was located and the abdominal wall was tented with forceps, allowing for a stab incision to be made using a 15# scalpel blade and extended using Mayo scissors. A Balfour retractor was placed to maintain the abdomen in an open position to allow for visualization during surgery.
The diaphragm was noted to have a large axial diaphragmatic hernia. Omentum, colon, cecum, ileum, and the majority of jejunum were located within the chest cavity and were easily replaced into the abdomen. The left lateral lobe of the liver was located within the pericardium as well, and the hernia was enlarged dorsally with sharp dissection to allow for reduction of the liver. The herniated liver lobe appeared mottled and dark red in color, with numerous areas of congested/abnormal tissue. Due to the presence of scare tissue, when the liver lobe was retracted into the abdomen, a hepatic vein was avulsed. Due to the severity of the damage to the liver lobe, and the bleed, a liver lobectomy across the hilus was performed utilizing a TA stapler with a 30 mm V3 cartridge and monopolar electrocautery.
Upon examination of the abdominal contents, the gallbladder was noted to be atrophied, and cystic and common bile ducts distended. The portal vein was also notably distended and there were numerous enlarged mesenteric lymph nodes.
An indwelling chest tube was placed between the 5th and 6th rib in routine fashion and confirmed in the thorax via palpation and direct visualization. It was then secured to the skin of the lateral thorax using 3-0 Ethilon suture.
The edges of the hernia were apposed using 2-0 PDS in a simple continuous pattern. The thoracic cavity was partially emptied of 300 mL of air via the chest tube, however positive pressure was intentionally left to prevent re-inflation injury to the lungs.
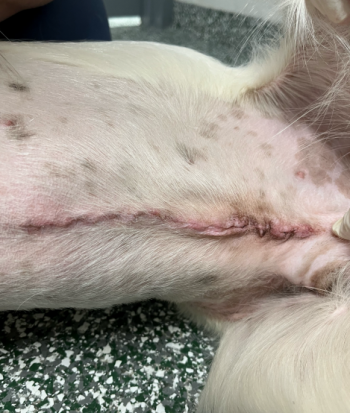
The abdominal cavity was lavaged with 1 liter of warm sterile saline and evacuated with a Poole suction tip. Closure was performed in a 3-layer manner. The linea was closed with 2-0 PDS in a simple continuous pattern. The subcutaneous tissues were closed with 3-0 Monocryl in a simple continuous pattern. Nocita was injected subcutaneously along the incision and the skin was closed with 3-0 Monocryl in a continuous intradermal pattern. The incision and surrounding tissue were cleaned using saline and an island dressing was placed.
Dom recovered well from anesthesia. Thoracic radiographs confirmed proper chest tube placement. He was maintained on IV fluids and pain management, and 10 mLs of air were removed from his chest tube every two hours post-op, in order to slowly re-inflate the lungs and prevent re-expansion pulmonary edema, a life-threatening complication seen with chronic diaphragmatic hernias.
The following day, Dom continued to improve and remain comfortable. When negative pressure was achieved, air no longer needed to be removed from his chest. He was transitioned to oral medications.
Two days post-operation, Dom was still doing well, and his chest tube was removed.
Notes
PPDH is a congenital disease in which a connection exists between the pericardium and the peritoneal cavity, which allows abdominal organs to move into the chest. It can be an incidental finding that causes no physical abnormalities. However, in cases like Dom's, the severity of the hernia and large number of abdominal organs within the chest cavity resulted in an inability to breathe, prompting the need for surgical correction.



